Main antibiotic-resistance pathogens classified by number of deaths (WHO, Nature).
Antibiotics: an ongoing war (part 6)
Antibiotic resistance is now a widespread and constantly expanding phenomenon, and can be mainly of two types: innate or acquired. In the first case, it is contained in the bacterium from its birth, while in the second is acquired during its life. This mechanism is possible by the ability of bacteria to exchange genetic material with other bacteria or to internalize genetic material found in the environment.
These phenomena are very complex, but we can simplify them as follow. Each bacterium has a large fixed DNA molecule, and a variable number of smaller circular DNAs separated from the first one, called plasmids. The large molecule, the chromosome, contains all the information for cell structure and metabolism, so it translates into proteins with many different functions. Besides that, there could also be information to produce proteins that degrade an antibiotic or prevent it from entering the cell and therefore acting. These proteins are responsible for antibiotic resistance, and their genes are often located in plasmids and thus exchanged between bacteria or lost outside in the environment during cell death. We could define them as upgrades for the bacterium; indeed, they can lend the most varied functions, not necessarily antibiotic resistance.
One of the main mechanisms of antibiotic resistance is represented by a mutation of the target molecule so that the antibiotic can no longer block its function. A second possibility is drug inactivation, which can occur through tiny modifications to the antibiotic operated by the cell. There are also proteins in the cell membrane that can make the bacterial wall impervious to antibiotics or transfer it outside the cell like actual pumps, lowering its concentration until making it harmless. Finally, bacteria can develop new processes to produce energy, as an alternative to a pathway blocked by a drug and thus manage to survive.
The spread of resistance from one pathogen to another, combined with the slow development of new antibiotics, kills an estimated 1.3 million people per year and is expected to grow to 10 million per year globally by 2050.
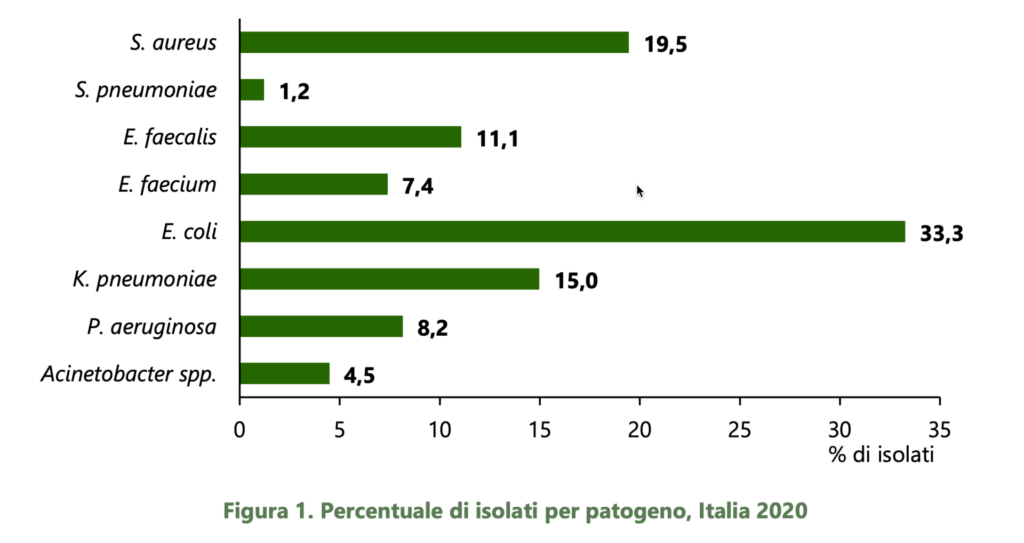
The image below shows the main species responsible for deaths caused by antibiotic resistance in Italy.